The Dramatic Degradation of the Human Immune System
In many countries worldwide over the past three and a half years the health and financial situation of the population has been falling downhill in a way that has never been seen in the past decades. Trend analysis shows increasing numbers of excess mortalities in all ages and a steep rise in a decay of people’s health and workability, especially women. Pandemic measures, repeated vaccinations and a rising number of people including children and pregnant women suffering from hunger have weakened people’s immune systems.
Impaired immune system conditions due to a disrupted gut microbiota and increased exposure to oxidative stress can stimulate S. pneumoniae to switch from a commensal bacterium to an opportunistic and harmful micro-organism that may result in pneumonia, myocarditis, cancer, neurodegenerative disease, and even sudden death.
To turn around the ongoing negative trend in health and life expectancy any forced ‘one-size-fits-all interventions’ that may cause a collapse of a weakened immune system need to be halted. Without any positive change in current public health policies, millions more adults and children will die from pneumonia and invasive pneumococcal disease in the next decades. No other infection can cause this number of deaths.
Instead, a safe, affordable, and effective intervention by a population-wide vitamin D supplementation, a known effective antioxidant and immunomodulator that can prevent dangerous pneumococcal infections is urgently needed.
In general, public health authorities and governments could better invest in and choose interventions that prevent malnutrition and extreme poverty. Strengthening the population’s immune system will decrease the demand for healthcare and contribute to a healthy world for all.
Trend analysis demonstrates the population’s weakening immune systems
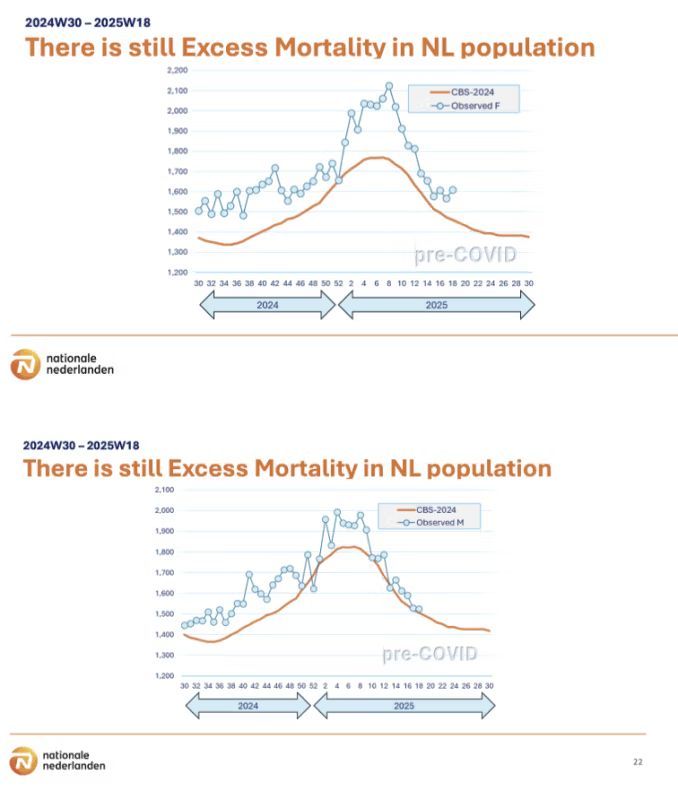
Worldwide data have shown a continued period of excess mortality as compared to pre-pandemic periods. According to the OESO covering a total of 1.2 billion inhabitants’ excess mortality in 2022 was 1.2 million. Reports of July 2023 show excess mortality continued to vary across the EU. Among them Sweden had the lowest excess deaths recorded.
A preprint study suggests that all-cause mortality during the first nine months of 2022 increased more the higher the 2021 vaccination uptake associated with monthly mortality increase in 2022 by 1,105 percent. Analysis of all-cause mortality rates in Japan and Germany found a highly significant increase from 5 and 10 percent in mortalities in 2021 and 2022 (2005-2022). For 96.5 percent excess mortality was seen in the vaccinated.
Interim analysis of Covid-19 vaccine effectiveness by the European Centre for Disease Prevention and Control described an apparent decrease in vaccine effectiveness for all age groups after 4 months of booster injection due to either the impact of waning immunity alone or to immune escape properties of a new Omicron variant. Recent data showed that the risk for infection increased with the number of injections with the Covid mRNA vaccines.
Whereas Covid-19 vaccines were meant to protect people with a weakened immune system for severe Covid-19, people with various diseases and on different medications reacted differently, depending on the medicine used and type of diseases. Most of the time people with a weakened immune system were advised to take more frequently repeated injections to respond better. Although, opinions on frequent booster vaccinations and how to proceed after Covid-19 infection differed widely in January 2022.
Also, the European Medicines Agency has warned that repeated Covid booster doses could adversely affect the immune response. Moreover, booster doses could contribute to viral mutations against the acquired immunity with higher transmissibility, leading to longer-term vaccine resistance and potential adverse effects on morbidity and mortality.
‘Vaccine exhaustion’ after repeated vaccination seems to be of increasing relevance to the Covid-19 pandemic. Although a steady decline in antibodies following Covid-19 vaccination is often used as a justification for repeated vaccination, the immunogenic effect of repeated vaccination depends on the age and the immune response of individuals. The same number of doses might be insufficient for some but excessive to others. As immunity acquired from Covid infection is as protective as vaccination against severe illness, concerns for booster vaccination about their effectiveness, sustainability, and possible dangers should be taken seriously.
For almost two years, peer-reviewed articles on how Covid-19 vaccines could destroy the immune system and cause harm often referred as Vaccine Acquired Immune Deficiency Syndrome (VAIDS) have been ignored.
Concerns on VAIDS support the reports from Phinance Technologies, with trend analysis on excess mortality, disabilities, and loss of productivity in the UK, the US, and Australia in 2021 – 2023. Deaths per 100k were trending down before 2020 and are trending up since 2020 with 3 deaths/100k higher than 2015-2019 for ages 15-44 years with highly statistically significant signals (black Swan events). Moreover, the rise in disabilities is trending up 4x more than deaths in 2022 from UK PIP for various chronic diseases including cancer and myocarditis. A worrying 2.6 million are out of the workforce due to long-term sickness in the UK. Increases in excess mortality on cardiovascular diseases aged 15-44 years were up 13 percent in 2020, 30 percent in 2021 and 44 percent in 2022. These strong data can no longer be ignored as next year a further increase can be expected.
The timeline report on Epoch Times on myocarditis and Covid-19 vaccines showed how the CDC missed a safety signal and hid a warning. An increasing number of peer-reviewed studies on myocarditis and pericarditis and even Sudden Cardiac Death after Covid-19 vaccination have been published. Even a cardiovascular assessment one year later shows a potential long-term effect of Covid-19 vaccine-associated myocarditis on exercise capacity and cardiac functional reserve during stress. A higher risk for myo/pericarditis cases was detected in those who received mRNA Covid-19 vaccinations compared with unvaccinated individuals in the absence of SARS-CoV-2 infection. Mild asymptomatic myocardial inflammation could be more common than ever expected. Moreover, recently the presence of mRNA vaccines has been detected in the heart up to 30 days from vaccination.
Even for children aged 0-14 years excess mortality is observed in the UK and EU countries from the second half of 2021. And Naomi Wolf recently reported that US maternal mortality increased sharply in 2021. A recent preprint showed the negative impact of Covid vaccines on pregnancy outcome and menstrual function. Post-vaccination neurological symptoms showed a substantial overlap with Long Covid symptoms.
While the past four years’ billions of tax money has been spent with the aim to protect the population from mortality or disease, official data show the opposite suggesting an ineffective, unsafe, and even harmful policy. Unfortunately, in several countries public authorities and governments have started to recommend a booster vaccination (6th injection) without informed consent. Even if analysis of a cohort of healthcare workers showed more absence due to side effects after a second injection, people are advised to take another booster. Moreover, the new Covid vaccine variant has not been tested in humans.
A possible relation of repeated Covid-19 mRNA injections with the downward trend on population’s health, workability, income, and life expectancy has not yet been investigated by Public Health Institutes and or communicated to the public. Remarkably, England JCVI said only at-risk groups and those aged 65 and over should be offered vaccines despite fears for overwhelming healthcare this winter.
Even when a paper on respiratory viruses acknowledged that current vaccines could not protect against infections and severe diseases, worldwide governmental flu and Covid-19 vaccine campaigns for the next autumn/winter season proceed, while recent obtained data from the CDC have now shown 77 percent of the hospitalized patients in 2020 did not have Covid as a primary cause.
The hidden role of Streptococcus pneumoniae in pandemics of respiratory viruses
In the context of a respiratory virus pandemic, it is important to acknowledge that a distinction between viral and bacterial infections is not clear in the literature. During the Covid-19 pandemic Acute Respiratory Distress Syndrome (ARDS) was wrongly presented as a new disease. For years ARDS or cytokine storm is known as a potential risk for people with a weakening immune system, especially during cold seasons. During viral infections coinfections with other pathogens, especially with Streptococcus pneumoniae have been reported repeatedly.
Pneumococcal infections were a major cause of influenza-associated pneumonia and death among both military persons and civilians in the 1918 pandemic. Eighty percent of pleural fluids of patients with pneumonia yielded bacteria.
Also during the H1N1 2009 influenza pandemic pneumococcal coinfection was found as the most common cause of death with 30 percent of patients without symptoms of pneumonia and 50 percent could only be diagnosed with an urinary antigen test. Pneumococcal coinfected patients showed a higher severity of disease with lower O2 saturation, higher acute phase serum levels, high humoral IgG4 subclass antibodies and more frequent admission to Intensive Care Units (ICU) indicating higher risks of mortality. Twenty-nine percent of the patients who died from infection with H1N1 influenza had evidence of bacterial infection with pneumococci predominantly of types not present in the pneumococcal conjugate vaccine.
Unfortunately, from the second half of 2021 studies in the UK, Switzerland, and Germany reported a reemergence of Community Acquired Pneumonia (CAP) by S. Pneumoniae in children younger than 15 years of age and elderly people, with higher coinfection rates as reported for influenza, and compared to the first period in the pandemic and pre-pandemic levels both in Covid-19 and non-Covid-19 CAP patients. This could portend an increase of pneumococcal infections across all age groups while coinfections with other non-Covid-19 viruses did not change. When viral and S. pneumoniae infections occur together, infections appear to be associated with severity of COVID-19 as well as poorer outcomes.
In many countries pneumococcal conjugate vaccine (PCV) is part of the governmental vaccination programmes for young children and elderly people. Unfortunately, effectiveness of the vaccines against secondary pneumococcal infections remains controversial. Residual disease caused by persistent vaccine type serotypes and non-vaccine serotypes remain substantial. Effectiveness varies by serotype and vaccine and PCV13 effectiveness was observed to decline with time after booster vaccination.
Moreover, the percentage of cases with underlying risk factors (chronic lung disease, cancer, heart disease. e.a.) increased by 50 percent in the late PCV13 period. Current pneumococcal vaccines confer incomplete protection against invasive pneumococcal disease (IPD). Several hundred variants of capsular serotypes complicate the development of effective vaccines and successful pneumococcus protein-derived vaccines have not yet become available. Growing levels of bacterial resistance have troubled effective treatments.
Clinicians need to have an increased awareness for coinfections or superinfections of viral infections with pneumococci, especially as CAP or IPD may continue to increase. Underestimation of pneumococcal CAP might occur because often a low sensitivity of the standard of care culture methods is used instead of the more accurate urinary antigen testing.
The importance of bacterial superinfection of the lung as a contributor to death in patients with Covid-19 has been underappreciated thus far. A study published in May 2023 found that pneumonia that does not resolve was a key driver in patients with Covid-19. Bacterial infections may even exceed death rates from the viral infection itself. The study highlighted the importance of preventing and looking for and aggressively treating secondary bacterial pneumonia in critically ill patients with severe pneumonia including Covid-19. Six months afterwards 60 percent of hospitalized patients showed abnormalities in multiple organs, especially the brain and lung and higher rates of heart-related risks including irregular heartbeats, heart attack, and stroke. In autopsy analyses a range of abnormalities, particularly in the way heart cells regulate calcium were found.
Long Covid symptoms, though still poorly defined, could be linked to a S. pneumoniae infection. Long-term mask-wearing could cause overgrowth of S. pneumoniae, which is a facultative anaerobic bacterium with increasing growth opportunities in low O2/ CO2 rich conditions.
Overall it is important to keep in mind that a latest age-stratified analysis found a much lower pre-vaccination Infection Fatality Rate of Covid-19 (0.03 – 0.07 percent) in the non-elderly population globally than previously suggested. Large differences were observed between countries and may reflect differences in comorbidities and other factors. It seems that ‘The biggest Public Health threat is not a virus but a weakening immune system.’
The opportunity for harmful behavior of Streptococcus pneumoniae in weakened immune systems
A possible role of a disseminated Streptococcus pneumoniae growth in relation to sudden death, myocarditis, pericarditis, skin problems, autoimmune diseases, and cancer has been described. Clinical signs, symptoms, and physical examination findings alone cannot distinguish S. pneumoniae disease from infections caused by other pathogens. The common resident in the upper respiratory tract is usually asymptomatic in healthy individuals. Higher carriage is found during winter seasons and often in crowded areas like childcare. While the overall attack rate of the pneumococcus is low, it is the leading cause of infectious deaths worldwide.
Infections primarily occur in the very young and old as their immune systems are underdeveloped or waning, respectively. Every year 12 million children are hospitalized for severe pneumonia requiring urgent oxygen treatment to survive. Pneumonia is concentrated in the most deprived and marginalized children with a poor nutritious status and a weakened immune system. At least one child dies from pneumonia every 39 seconds, which is 800,000 per year and accounts for more deaths than any other infectious disease worldwide. Sudden death in infancy has been related to bacterial infections. A systematic review observed a dose-response relation of sudden unexpected death and socioeconomic status.
Unfortunately, malnutrition and the threat of famine worldwide is rising. A recent UN report on the direct and indirect effects of Covid-19 pandemic and response said it killed 228,000 children in South Asia and a sharp increase of more than 20 percent in maternal deaths.
Especially elderly people and immunocompromised individuals are at increased risk for developing Invasive Pneumococcal Disease (IPD), when the bacteria spreads from the nasopharynx to other parts of the body including the lungs, blood, and brain. Once in the bloodstream pneumococci disseminate widely into many organs where the bacteria can bind.
While much has been written on pneumococcal pneumonia, recent studies have shown that S. Pneumoniae is able to invade the myocardium and kill cardiomyocytes. One in five persons with pneumonia in hospital experience cardiac complications and for those with pneumococcal bacteremia adverse cardiac events in convalescence is a risk factor for up to ten years. The interactions between pneumococcus and the heart are an emerging field.
The virulence determinants of the pneumococcus that mediate the greatest inflammation and cytotoxicity are the pneumococcal cell wall, pneumolysin, hydrogen peroxide, and some other secreted products like peptidoglycan. The cell wall of the pneumococcus is inhibitory for cardiac contractility. The pneumococcus toxin, pneumolysin, has multiple interactions with the host leading to extensive spread of disease, intense inflammation, abundant cell damage, and necrosis, decreasing the bactericidal function of mast cells and the opportunity for bacteria to cross into the bloodstream.
Pneumolysin disrupts Ca2+ signalling due to pore formation even if cells are not immediately killed. The effects of hydrogen peroxide contribute to mitochondrial damage of neurons and cardiac damage. Hypoxia and hypotension with arrhythmia, myocardial infarction, myocarditis, pericarditis, and congestive heart failure can be found. Cardiac complications may occur because of poor oxygenation status at a time of increased myocardial demand and/or because of unintended effects of antimicrobials or other medicine.
Pneumococcal bacteremia with metastatic infection and meningitis is responsible for significant mortality, particularly in the elderly where rates may be as high as 60 percent and 80 percent respectively. The bacteria are also known as a contributor to end stage renal disease in both children and adults.
People that survive pneumococcal meningitis often experience permanent neurological sequelae with defects in memory and learning because of neuronal damage by pneumolysin and hydrogen. If the pneumococcus enters the middle ear, the pneumolysin strongly contributes to cochlear damage and hearing loss. Bacterial products encountered during pregnancy may be associated with cognitive disorders in children.
Diversity gut microbiota protective in infections and vaccine side effects
The influence of gut microbiota on a diminished capacity to phagocytose and killing by alveolar macrophages of S. pneumoniae was demonstrated in a study with microbiota depleted mice. Findings of the study support the protective role of the gut microbiota against organ failure during S pneumoniae induced sepsis. Alveolar macrophages are thought to be the first line of defense in case of pathogen invasion towards the lung. Gut microbiota has been shown to regulate immune defenses against infection of the upper respiratory tract
with influenza A virus. The role of the gut microbiota became even more evident by a report that described successful treatment with lactobacillus rhamnosus in critically ill patients with ventilator associated pneumonia. Probiotic prophylaxis was also effective to prevent ventilator associated pneumonia in children on mechanical ventilation.
Large communities of intestinal microbes not only contribute to a local host defense against infections but also modulates responses at systemic sites. Mice depleted with microbiota before infection with S Pneumoniae showed enhanced liver and hepatic injury. A difference in microbiota composition in the Upper Respiratory Tract between young and elderly mice showed more diversity in young mice and faster clearance to baseline.
Risk for invasive pneumococcal disease is much higher for patients with inflammatory bowel disease or other comorbidities and/or use of multiple medicines that modulate the gut microbiota. In older hospitalized patients polypharmacy but not multimorbidity and frailty was significantly associated with gut dysbiosis. The severity of dysbiosis was able to significantly predict death after a two-year follow-up. An English Longitudinal Study on Ageing found that older adults with polypharmacy were at higher risk of all-cause mortality and mortality due to cardiovascular diseases as compared with those who did not take medication.
Recent studies indicate that dysbiosis of the gut microbiota is thought to be the cause of most cardiovascular diseases, including coronary heart disease, hypertension, arrhythmias, heart failure, and sudden cardiac death. Gut microbiota dysbiosis can induce an inflammatory response and affect the metabolism of bioactive molecules, resulting in systemic inflammation and endothelial dysfunction. These changes promote the development of artherosclerotic plaques and increase the risk of thrombosis and cardiovascular events.
A decline in biodiversity of the gut microbiota in the genus Bifidobacteria is observed with inflammatory bowel disease, obesity, neurological disorders C. Difficile infection, and recently severe Covid-19 infection (ARDS). Patients with severe SARS-CoV-2 infection possess significantly less bacterial diversity with lower abundance of Bifidobacterium and Faecalibacterium and increased abundance of Bacteroidetes as compared to those with lighter symptoms.
A direct association was observed between severity of Covid-19 disease and Bacteroides abundances. A large cohort from the US showed that digestive symptoms were associated with patients that showed 70 percent risk of testing positive for SARS-CoV-2. Patients with GI manifestations like diarrhea were related to longer disease duration.
Preliminary data showed a persistent damage to the gut microbiome with a decrease in Bifidobacterium following the messenger RNA SARS-Cov-2 vaccine. The decline in Bifidobacterium after vaccination might explain the higher risk for a SARS-CoV-2 infection after each mRNA booster injection. Analysis of US nursing homes data proves the vaccine made it more likely for the elderly to die. A recent study with the BNT162b2 Covid vaccination in children observed altered cytokine responses to heterologous pathogens that can persist up to six months after vaccination. However, it is not clear whether these changes provide protection against other infectious diseases.
Studies suggest there is a bidirectional relationship between the gut microbiota and the Covid-19 vaccine and the varying components of the microbiota either enhancing or reducing the vaccine efficacy. Unfortunately, recent UK numbers showed that 96.5 percent of excess mortality occurred in vaccinated individuals.
Food insecurity and malnutrition may be linked to microbiota immaturity and/or dysbiosis. The nutritional status may affect Covid-19 vaccine efficacy by modulating the immune system and influencing inflammations and oxidative stress. With many people facing a weakened immune system, disrupted microbiota, and increased oxidative stress any ill-considered intervention could be fatal by a final toxic attack of Streptococcus pneumoniae on the body’s immune system.
A threatening food insecurity worldwide due to war and climate change policies will exacerbate the risk for severe infectious and chronic diseases. During the pandemic the number of people and children in extreme poverty rose from 70 million to 700 million. Moreover, collapsing healthcare systems will not be able to cover a demand for increased care and rising numbers of morbidity and mortality.
Continuing the same policies will make the UN Decade for Healthy Ageing 2020-2030 and Zero Hunger in 2030 a farce and will maximize public distrust.
The urgent need for a population wide Safe Affordable Effective Intervention
At the start of the pandemic the scientific literature on the protective effects of Vitamin D3 for prevention of seasonal pneumonia and Acute Respiratory Distress Syndrome has been ignored and disputed by many medical doctors, scientists, experts, and politicians with the argument that more research would be needed before general recommendations can be made. However, cost-effective harm analysis shows even a small decrease in infections could justify such an intervention.
Data from Israel, Spain, and Belgium showed that low vitamin D plasma 25(OH)D levels appear to be an independent risk factor for Covid-19 infection, and hospital mortality. Patients with vitamin D deficiency had greater prevalence of raised biomarkers for cardiovascular diseases.
Vitamin D deficiency with a 25(OH)D concentration below < 30 nmol/l should be avoided wherever possible as it dramatically increases the risk of excess mortality, infections, and many chronic diseases i.e pneumonia, sepsis, cardiovascular disease, cancer, diabetes, muscle, and bone health. In some countries approximately 80 percent of individuals are affected by vitamin D deficiency. Around 66 million people in the EU show serum vitamin D levels < 50 nmol/l. Hypovitaminosis of vitamin D impairs mitochondrial functions and enhances oxidative stress and systemic inflammation. Vitamin D deficiency has been linked with gut dysbiosis and inflammation and associated with worse outcome of diseases. A synergistic effect of vitamin D3 and Bifidobacterium has been demonstrated in reducing the severity of bacterial and viral infections via suppression of inflammatory responses and blocking translocation of bacteria.
Unfortunately, up to now nothing has changed to protect the global population from vitamin D deficiency despite the consensus that vitamin D has a host of immunomodulatory effects which may be beneficial in the context of Covid-19 and low levels of vitamin D can result in dysfunction of crucial antimicrobial effects. Vitamin D deficiencies predispose children to respiratory infections.
Recent studies demonstrated the crucial role of vitamin D above 50 nmol/l at all times a year in protection against pneumonia or ARDS and prevention of hospitalization, with better protection than Covid-19 vaccination or flu vaccination and with less side effects. A protective role of vitamin D supplementation in the regime of patients with Covid-19 was indicated. Vitamin D supplementation given at a daily maintenance as an antioxidant and immunomodulator may prove a relative simple applicable intervention to modify an important risk factor for a waning immune system, beneficial in improving resistance to overall respiratory infections by S. pneumoniae, and/or SARS-CoV-2 virus variants and/or pathogen X.
In face of new winter seasons with an increased risk for ARDS and a collapsing healthcare system, a strategic investment and support in the health of citizens all times a year with protective vitamin D serum levels (at least 50-100 nmol/l) is a safe, affordable, and cost-effective investment. This will be a much safer and effective way forward to contribute to a world with healthy aging, zero hunger and reducing pneumonia.
Author: dr. Carla Peeters
First published at Brownstone Institute